Coatings are perhaps best known for protecting and beautifying surfaces on structures like bridges, ships, manufacturing plants, commercial buildings, and homes. However, they are equally important for the functionality they impart to many other lesser known applications, such as those in the pharmaceutical industry. Two recent developments from the Wyss Institute for Biologically Inspired Engineering at Harvard University underscore the potential for novel coating technologies to help save patient lives.
The first coating is designed to prevent infectious biofilm formation on implanted medical devices. Such device-associated infections can affect the performance of implanted devices and also contribute to the rapid increase in antibiotic resistance, according to Wyss researchers. The new coatings were developed by Joanna Aizenberg, a Wyss Institute Core Faculty member, Professor of Chemistry and Chemical Biology, and the Amy Smith Berylson Professor of Materials Science at the Harvard John A. Paulson School of Engineering and Applied Sciences (SEAS) and Elliot Chaikof, who is also with the Wyss Institute and SEAS and the Beth Israel Deaconess Medical Center. The coatings are self-healing slippery surfaces based on medical-grade Teflon materials and liquids that prevent biofilm formation on medical implants. At the same time, they preserve normal, innate immune responses against pathogenic bacteria.
The SLIPS (slippery liquid-infused porous surfaces) coating technology was initially developed by Aizenberg, who was inspired by the carnivorous Nepenthes pitcher plant. The plant uses the porous surface of its leaves to immobilize a layer of liquid water, creating a slippery surface for capturing insects. Aizenberg’s group has previously created coatings that repel ice, crude oil, and biological materials on surgical and diagnostic instruments. By tuning the chemical and physical properties of the coatings through the choice of medical-grade polymeric material and infused lubricant, the researchers are developing systems with carefully designed nonfouling properties under specific conditions and in specific environments. The new advance in this case is the use of medical- grade Teflon, which is widely used for implanted medical devices, according to Aizenberg.
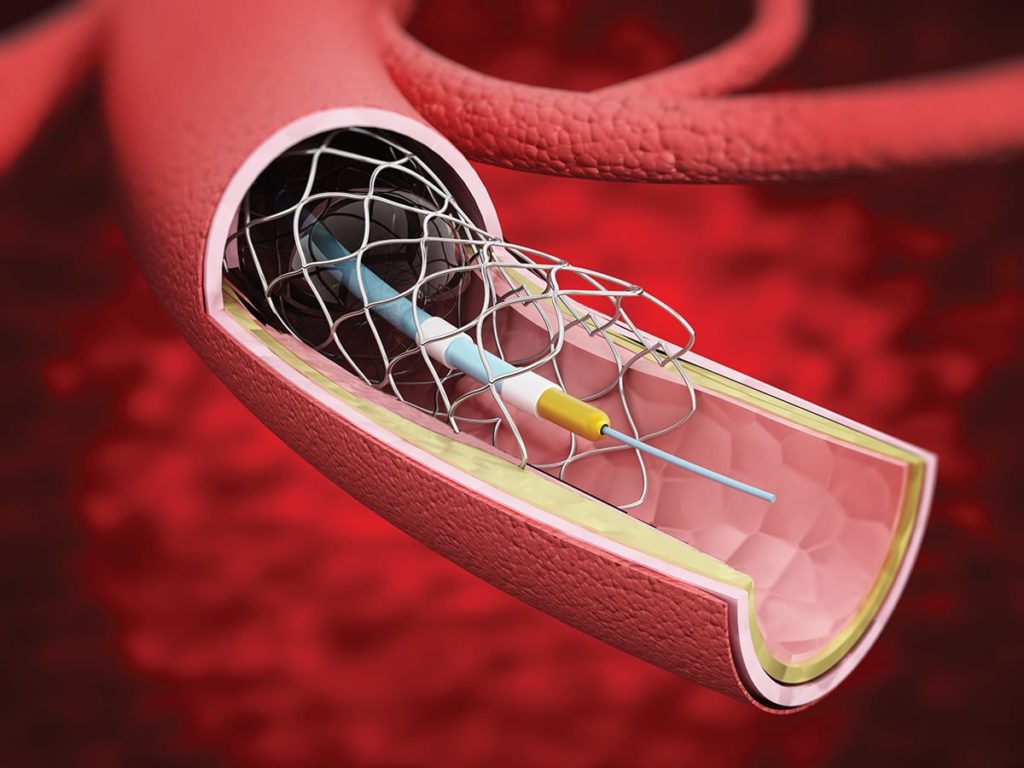
The research first sought to identify the right combination of Teflon and lubricant that would repel the most common device-associated bacterial strain and yet preserve the anti-bacterial activity of innate immune cells that provide the natural first-line response against invading bacteria. These investigations were performed ex vivo. Expanded polytetrafluoroethylene (ePTFE), which is used in grafts for cardiovascular reconstruction, mesh for hernia repair, and reconstructive surgery implants, provided the best results. The performance of coated and noncoated hernia meshes implanted in mice infected with Staphylococcus aureus was then evaluated. Rewardingly, the SLIPS coatings resisted infections and were associated with considerably less infiltrating immune cells and inflammatory abscesses than noncoated ePTFE, according to Chaikof. He noted that the use of SLIPS coatings on implanted devices could potentially obviate the need for treatment with antibiotics at the time of implantation.
. . . Researchers envision that their method can improve cell-based therapies, help explore heterogeneity between cell populations that underlie tumors and other abnormalities, and even enable a paradigm shift in precision tissue engineering
The second development involves the encapsulation of single cells within tunable microgels, allowing greater control at the cellular level. Researchers from the Wyss Institute and SEAS have introduced a highly effective microfluidic method for encapsulating single cells in microscale hydrogels, allowing for the exertion of much greater specificity of control upon cells and increasing their ability to survive implantation. Alginate hydrogels are attractive for medical applications because of their biocompatibility and the ability to tune their mechanical and biochemical properties to match physiological conditions. They have previously been demonstrated to influence the differentiation of stem cells, incite immune attacks on cancer cells, and weaken the resistance of tumors to chemotherapy, but through the control of groups of cells.
The new technology allows researchers to influence cell behavior at the single-cell level, according to David Mooney, a Wyss Core Faculty member and the Robert P. Pinkas Family Professor of Bioengineering at SEAS. The single cells can also be used as building blocks for larger cell structures, according to David Weitz, the Mallingkrodt Professor of Physics and Applied Sciences at Harvard University and SEAS. The key advantage of the microfluidic method is the production of very thin hydrogel layers around each cell. Unlike existing technology where only 4% of the capsule volume is accounted for by cells in rather large capsules, the new method provides encapsulated cells in which the cell accounts for 40% of the volume in much smaller capsules. The smaller size allows for intravenous delivery, thus creating new formulation opportunities for cell-based therapies and potentially allowing more rapid delivery of these treatments. The protective hydrogel layer may also enable cells to survive longer in the body; microgels infused with growth and anti-inflammatory factors could delay attack by the immune system.
The process involves first coating the cells with calcium carbonate nanoparticles to facilitate cell encapsulation when mixed in an alginate polymer solution. Unlike conventional approaches, however, the researchers then washed the cells to remove non-adherent nanoparticles using a water and oil emulsion inside a microfluidic device. As a result, microgel-encapsulated single cells are the predominant product. Notably, the process is rapid, with 1,000 cells encapsulated each second.
The researchers envision that their method can improve cell-based therapies, help explore heterogeneity between cell populations that underlie tumors and other abnormalities, and even enable a paradigm shift in precision tissue engineering.